Reviewed by Dr. Karan Raj Jaggi
Dr. Karan Raj Jaggi is a triple board-certified, internationally trained orthopaedic surgeon super-specialising in regenerative orthopaedics, sports injuries and fast-track joint replacements.He currently serves as the Chief Medical Officer and Head, Regenerative Orthopaedics at Osso Orthopaedic Centres, where he leads cutting-edge orthopaedic care with a focus on holistic, patient-centric treatments.
February 3, 2026
Joint pain, particularly in the knee, represents one of the most common complaints in orthopaedic practice. The decision between pursuing regenerative therapies versus proceeding with knee replacement surgery deserves careful consideration.
For decades, total knee replacement has been positioned as the definitive only solution for advanced joint degeneration. While arthroplasty certainly has its place, the emergence of regenerative medicine has fundamentally changed how we approach patients who fall into that grey zone between conservative management and surgical intervention.
Understanding the Spectrum of Knee Degeneration
Not every patient with knee pain requires surgery. Understanding where you fall on the spectrum of joint degeneration helps you have a more informed conversation with your orthopaedic surgeon, though only a thorough clinical evaluation can determine the right treatment path for your specific condition.
Osteoarthritis develops progressively, beginning with cartilage softening and advancing through various stages until bone-on-bone contact occurs. The critical point: many patients present somewhere in the middle stages, where the joint is damaged but not destroyed.
The Kellgren-Lawrence grading system classifies osteoarthritis from Grade 1 (doubtful narrowing with possible osteophytes) through Grade 4 (large osteophytes, severe narrowing, definite bone deformity). Patients in Grades 2 and 3 often represent ideal candidates for regenerative intervention because their joints retain enough biological potential to respond to treatment.
What Is Regenerative Medicine for Joints?
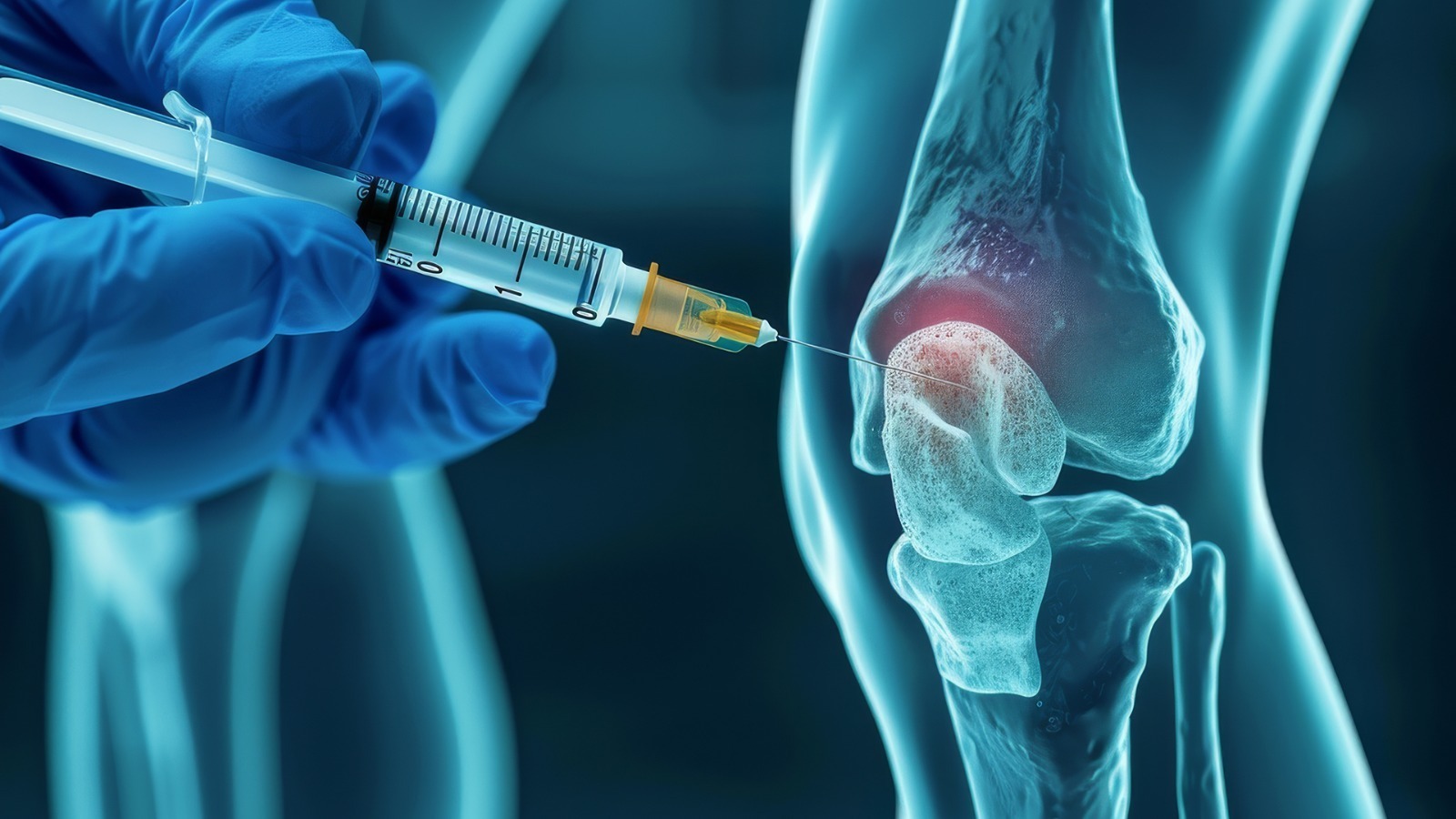
Regenerative medicine encompasses therapies designed to stimulate your body’s natural healing mechanisms rather than replacing damaged structures with artificial components.
- Platelet-Rich Plasma (PRP) concentrates growth factors from your own blood and delivers them directly to the damaged joint, promoting tissue repair and reducing inflammation.
- Growth Factor Concentrate (GFC) provides higher concentrations of specific growth factors associated with tissue regeneration while eliminating inflammatory components.
- Hyaluronic acid injections restore joint lubrication and shock absorption, supplementing the viscous fluid that healthy joints produce naturally.
Read also: Acute vs Chronic Sports Injuries: What’s the difference?
When does regenerative medicine make sense for joint pain?
A thorough clinical evaluation by an orthopaedic specialist is essential before considering regenerative therapy. Your doctor will assess multiple factors, including imaging, physical examination, medical history, and lifestyle, to determine whether you’re a suitable candidate for this approach.
- Early to moderate osteoarthritis responds most favourably because the joint retains sufficient healthy tissue to participate in the healing response. Severely degenerated joints lack the biological substrate necessary for regeneration.
- Younger patients deserve special consideration. A knee implant has a finite lifespan of 15–20 years, meaning a patient undergoing surgery at age 50 will likely require revision during their lifetime. Regenerative therapies can potentially delay that first replacement by years.
- Active individuals should understand that total knee replacement comes with permanent activity restrictions. Modern implants tolerate more activity than previous generations, but they are not designed for running, jumping, or high-impact sports.
- Patients with localised damage rather than diffuse joint destruction often respond excellently, particularly when damage affects one compartment while adjacent areas remain preserved.
- Those who have failed conservative treatment but are not yet surgical candidates occupy a treatment gap that regenerative medicine fills effectively.
Dr Karan Raj Jaggi’s Perspective
“Regenerative orthopaedics is not about avoiding surgery at all costs. It is about appropriate patient selection and timing. A 52-year-old executive with moderate cartilage loss and an active lifestyle is a completely different clinical scenario from a 72-year-old with bone-on-bone arthritis who struggles to walk to the bathroom. The goal is always to match the right treatment to the right patient at the right time.”
Read also: PRP Injections for Knee Osteoarthritis: what to expect?
When does joint replacement become necessary?
Despite advances in regenerative orthopaedics, knee replacement remains the appropriate choice for many patients.
- Bone-on-bone arthritis with complete cartilage loss leaves no biological tissue for regenerative therapies to work with. These patients typically experience dramatic improvement from arthroplasty.
- Significant joint deformity that alters the mechanical axis requires surgical correction. Regenerative therapies cannot address underlying structural problems, and malalignment will continue driving degeneration.
- Failed regenerative therapy after an adequate trial indicates the joint has progressed beyond biological approaches. Proceeding to replacement becomes the logical next step.
- Severe functional limitation preventing basic daily activities warrants surgical consideration. When pain prevents walking, sleeping, or essential activities, the risk-benefit calculation shifts toward intervention.
Realistic Expectations: What Each Approach Delivers
Regenerative therapies aim to reduce pain, improve function, and slow disease progression not cure arthritis or regrow cartilage to a pre-disease state. Most patients undergoing PRP or GFC experience 40–70% pain reduction with effects lasting anywhere between 6 months to 2-3 years, depending on the condition of the joint. Treatment can be repeated without cumulative risks.
Total knee replacement delivers more predictable and complete pain relief in appropriately selected patients. Studies demonstrate 85–90% report significant improvement, though 10–15% experience persistent pain despite technically successful procedures. Recovery extends 3–6 months before returning to normal activities.
The Disadvantages of Joint Replacement Worth Considering
Irreversibility stands as the most significant consideration. Once your native joint is removed, any future problems must be addressed through revision surgery.
Activity limitations persist permanently. While you can expect to walk, cycle, swim, and play golf comfortably, impact activities, pivoting, and deep flexion remain restricted.
Recovery time extends longer for elderly patients. The physiological stress of surgery combined with rehabilitation demands can prove challenging.
Potential complications, including infection, blood clots, implant loosening, and persistent pain, occur in a minority but represent real risks.
Implant longevity concerns anyone undergoing replacement at younger ages. Revision surgery carries higher complication rates and typically delivers inferior outcomes.
Read also: How Is Regenerative Medicine Changing ACL Injury Recovery?
A Framework for Decision-Making
When evaluating whether regenerative therapy or joint replacement is more appropriate, your orthopaedic specialist considers several key factors: the stage of arthritis and remaining joint space, your age, activity level and lifestyle demands, whether conservative treatments have been adequately tried, and your personal goals for treatment. Understanding this framework helps you have a more informed conversation with your doctor and ensures all relevant factors are considered in your treatment plan.
Consider knee replacement if: you have bone-on-bone arthritis with complete cartilage loss, you have failed adequate trials of conservative and regenerative treatment, your pain significantly limits daily activities, or you have realistic expectations about post-surgical activity levels.
The Role of Comprehensive Evaluation
The decision between regenerative medicine and joint replacement should never rest on imaging alone. A comprehensive evaluation considering symptoms, functional limitations, activity goals, and overall health provides the foundation for individualised recommendations.
At OSSO, we approach each patient, understanding that appropriate treatment for one person may be premature intervention for another. The goal is to match the right treatment to the right patient at the right time.
Your joints carried you this far. They deserve thoughtful evaluation before any irreversible decisions are made.
Frequently Asked Questions about ACL Tear in Gurgaon
At what age is knee replacement not recommended?
There is no absolute age cutoff. However, younger patients (under 55–60) are often encouraged to explore regenerative options first, as implants have finite lifespans and revision surgery carries higher risks.
Can regenerative medicine cure my arthritis?
No. Regenerative therapies reduce pain, improve function, and may slow progression, but they do not cure osteoarthritis or restore cartilage to its original state.
How do I know if I am a candidate for regenerative therapy?
A thorough clinical evaluation is essential by an orthopaedic surgeon. Patients with Kellgren-Lawrence Grade 2–3 osteoarthritis, preserved joint space on imaging, and realistic expectations typically respond best.
What if regenerative treatment does not work for me?
Joint replacement remains available. Trying regenerative approaches does not compromise future surgical outcomes.
How long can regenerative therapy delay knee replacement?
This varies significantly. Some patients delay surgery by 2–5 years, others by a decade or more. However, this typically requires a series of regenerative injections over the years, not a single treatment. Disease progression, activity level, individual biology, and commitment to ongoing maintenance sessions all influence outcomes.
Is regenerative medicine just delaying the inevitable?
For some patients with progressive disease, yes. But delaying replacement, especially in younger patients, means receiving a more advanced implant later and potentially avoiding revision surgery entirely.