Reviewed by Dr. Karan Raj Jaggi
Dr. Karan Raj Jaggi is a triple board-certified, internationally trained orthopaedic surgeon super-specialising in regenerative orthopaedics, sports injuries and fast-track joint replacements.He currently serves as the Chief Medical Officer and Head, Regenerative Orthopaedics at Osso Orthopaedic Centres, where he leads cutting-edge orthopaedic care with a focus on holistic, patient-centric treatments.
February 9, 2026
When joint pain begins affecting daily function, treatment becomes necessary. The question shifts from whether to treat, to which treatment pathway makes the most sense.
Making that decision requires looking beyond the hospital bill. Recovery downtime, lost productivity, and long-term restrictions carry significant weight often exceeding direct medical expenses. This blog provides a detailed comparison of joint replacement surgery, prolonged physiotherapy, and regenerative medicine to help patients evaluate their options comprehensively.
The Hidden Costs Nobody Talks About
Downtime Is the Cost Most Patients Underestimate
When evaluating orthopedic treatment options, most people focus on the hospital bill. But the real financial hit often comes from what you can’t do while recovering. A working professional earning ₹1.5 lakhs per month faces ₹4.5-9 lakhs in lost income during 3–6 months of surgical recovery. That’s often more than the surgery itself. For business owners, stepping away for months can mean lost clients, missed deals, and operational disruptions that don’t show up on any medical bill. For parents, it means weeks of depending on others for school runs, household responsibilities, and basic caregiving. Downtime isn’t just inconvenient. It’s expensive.
Joint replacement surgery requires 3-6 months before returning to normal activities. The first 6-8 weeks involve significant mobility restrictions, walker or crutch dependence, and inability to drive. You’re not just recovering, you’re on pause.
Endless physiotherapy without addressing the underlying problem often stretches across years. Three sessions weekly, indefinitely, while pain persists and function gradually declines. The cumulative hours lost to clinic visits add up. So does the mental burden of managing chronic pain with no clear end in sight, and the activities you quietly stop doing because they’ve become too difficult.
Regenerative orthopedic treatment typically involves 1–3 clinic visits with 48–72 hours of reduced activity. Most patients return to work within days. The contrast isn’t marginal. It’s measured in months versus days.
When you factor in lost income, missed opportunities, and the life you put on hold during recovery, the cheapest treatment on paper isn’t always the cheapest treatment in reality.
Also read: How Is Regenerative Medicine Changing ACL Injury Recovery?
Comparing Treatment Pathways
Surgery + Post-Op Rehabilitation
What it involves: Hospital admission, anaesthesia, joint replacement procedure, 3–5 day stay, 3–6 months rehabilitation.
Best for: Bone-on-bone arthritis (Grade 4), failed conservative treatments, severe functional limitation.
True costs:
- Direct: ₹5-6+ lakhs (surgery, hospital, rehabilitation)
- Downtime: 3-6 months significantly impaired
- Long-term: Activity restrictions, potential revision surgery in 15–20 years
Benefits: Predictable, significant pain relief in 85–90% of appropriately selected patients. Definitive solution for end-stage disease.
Physiotherapy
What it involves: Ongoing sessions (2–3 weekly), exercises, pain management, and activity modification.
Best for: Mild symptoms, post-injury recovery, surgical preparation or avoidance.
True costs:
- Direct: ₹2.5-4.5 lakhs over 2 years
- Downtime: Continuous time investment without resolution
- Long-term: Disease may progress while symptoms are managed
Benefits: Non-invasive, builds strength, improves function. But for degenerative conditions, often manages rather than resolves.
Also read: Common Sports Injuries: Prevention, Treatment, and Recovery
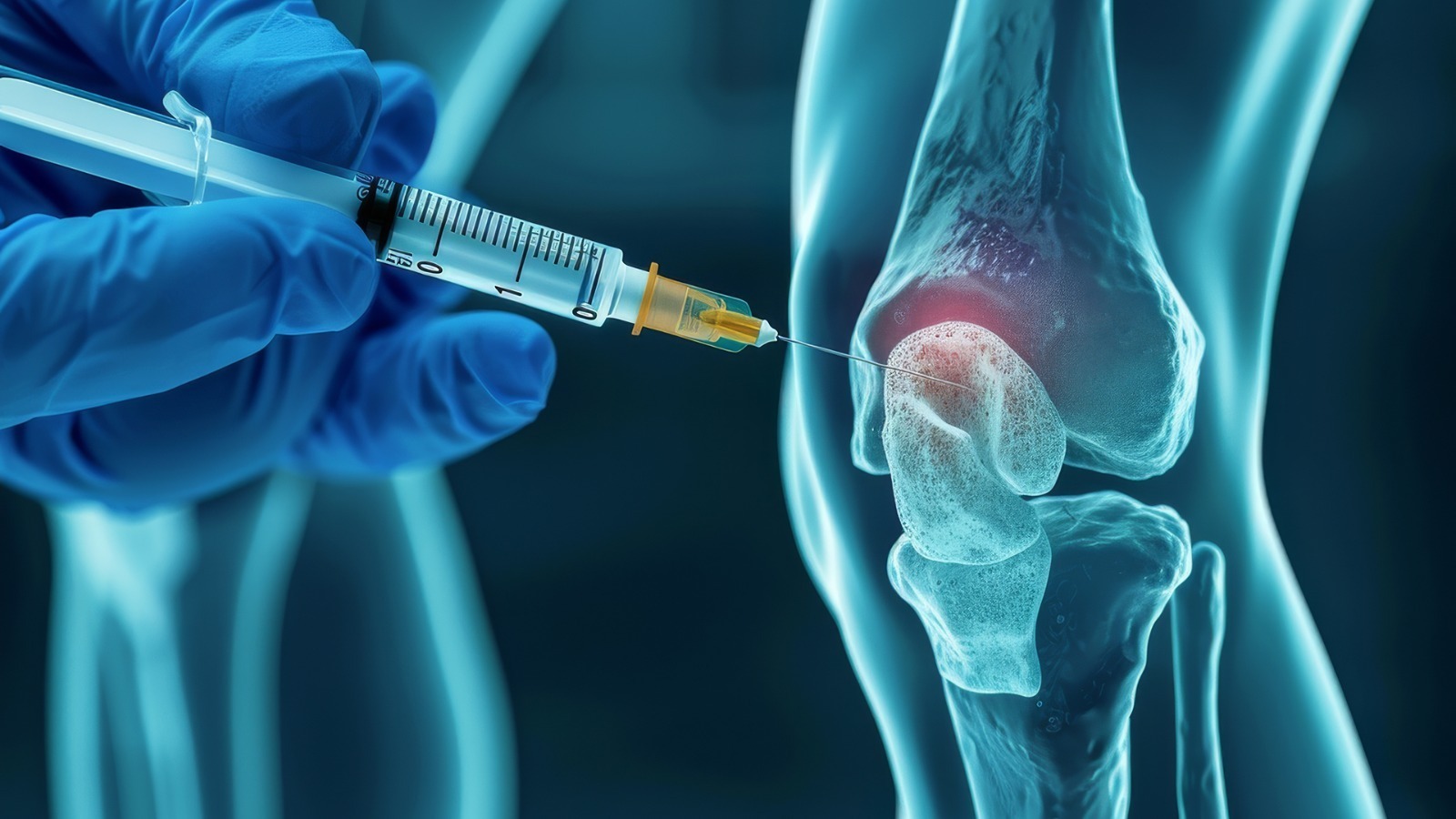
Regenerative Orthopaedic Treatment
What it involves: Minimally invasive injection-based therapy, PRP therapy, stem cell treatment, GFC therapy, viscosupplementation, or prolotherapy, depending on the condition.
Best for: Early to moderate osteoarthritis, tendon healing, ligament repair, cartilage regeneration, rotator cuff tears, meniscus tear treatment, and sports injury recovery.
True costs:
- Direct: ₹30,000–2.5 lakhs, depending on therapy
- Downtime: 2–7 days of reduced activity
- Long-term: May need repeat treatment; preserves surgical options
Benefits: Tissue regeneration rather than symptom suppression. Natural healing using autologous cell therapy. Accelerates healing. Minimal life disruption. Avoids or delays joint replacement.
When Regenerative Treatment Gives the Best Value
Regenerative medicine offers the strongest cost-benefit ratio for:
- Working professionals who cannot afford months away from their careers. The alternative to knee replacement surgery makes economic sense when downtime costs exceed treatment costs.
- Active individuals are unwilling to accept permanent activity restrictions. Joint restoration through biologic treatment preserves the ability to run, play sports, and live without movement limitations.
- Younger patients (under 60) face the prospect of revision surgery if they replace joints too early. Delaying replacement by even 10 years with non-surgical orthopedic treatment can mean avoiding revision entirely.
- Early-stage osteoarthritis, where cartilage repair and musculoskeletal regeneration remain possible. Waiting until bone-on-bone disease develops eliminates regenerative options.
- Tendon and ligament injuries where soft tissue repair through orthobiologics can restore function without surgical intervention.
When Surgery Makes More Sense
Regenerative treatment is not appropriate for everyone. Joint replacement delivers superior value when:
- Complete cartilage loss leaves no tissue for regeneration
- Severe deformity requires structural correction
- Pain prevents basic daily activities despite adequate regenerative trials
- Patient goals align with post-surgical activity expectations
Also read: PRP Injections for Knee Osteoarthritis: what to expect?
The Bottom Line
Regenerative orthopedic treatment is the right choice, but for those with early to moderate joint disease, tendinopathy, or sports injuries those who value their time and activity level, the cost-benefit analysis frequently favours biologic treatment over surgical intervention or indefinite physiotherapy.
The question is not whether you can afford regenerative medicine. It is whether you can afford not to consider it.
At OSSO, we help you evaluate all your options, surgical and non-surgical, so you can make an informed decision based on your condition, goals, and lifestyle. Book a consultation to understand which treatment pathway makes the most sense for you.
Frequently Asked Questions
- Is PRP therapy covered by insurance?
Most insurance policies in India do not cover regenerative treatments as they are considered advanced therapies. However, the out-of-pocket cost often compares favourably to surgery when total expenses are calculated. - How many regenerative treatment sessions will I need?
Typically, 1-3 sessions spaced 4-6 weeks apart. Some patients require annual maintenance. Your orthopaedic specialist will recommend a protocol based on your condition. - Can I return to work immediately after PRP or stem cell therapy?
Most patients return to desk jobs within 1–2 days. Physically demanding work may require 5–7 days of modification. - What if regenerative treatment does not work?
Surgery remains available. Trying regenerative approaches does not compromise future surgical outcomes and may provide valuable months or years of improved function. - How do I know if I am a candidate?
Patients with Grade 2–3 osteoarthritis, tendon injuries, ligament damage, or early degenerative changes typically respond best. A comprehensive evaluation determines candidacy.
Frequently Asked Questions about ACL Tear in Gurgaon
At what age is knee replacement not recommended?
There is no absolute age cutoff. However, younger patients (under 55–60) are often encouraged to explore regenerative options first, as implants have finite lifespans and revision surgery carries higher risks.
Can regenerative medicine cure my arthritis?
No. Regenerative therapies reduce pain, improve function, and may slow progression, but they do not cure osteoarthritis or restore cartilage to its original state.
How do I know if I am a candidate for regenerative therapy?
A thorough clinical evaluation is essential by an orthopaedic surgeon. Patients with Kellgren-Lawrence Grade 2–3 osteoarthritis, preserved joint space on imaging, and realistic expectations typically respond best.
What if regenerative treatment does not work for me?
Joint replacement remains available. Trying regenerative approaches does not compromise future surgical outcomes.
How long can regenerative therapy delay knee replacement?
This varies significantly. Some patients delay surgery by 2–5 years, others by a decade or more. However, this typically requires a series of regenerative injections over the years, not a single treatment. Disease progression, activity level, individual biology, and commitment to ongoing maintenance sessions all influence outcomes.
Is regenerative medicine just delaying the inevitable?
For some patients with progressive disease, yes. But delaying replacement, especially in younger patients, means receiving a more advanced implant later and potentially avoiding revision surgery entirely.